Giving Yourself for Parts
Every year over 5000 people in Ukraine need organ transplants. Of them, 2500 are waiting for new kidneys, 1500 for livers, and over 1000 for hearts. Yet only 130 such operations are conducted annually. And this despite the fact that the world’s first-ever kidney transplant was attempted in Ukraine in 1933. Neighbors in Belarus and Russia have already built up a transplant system—citizens there are saved according to need as organs are found. But Ukrainians who want an allogeneic transplant (from a non-related donor) have to go to India, Turkey, or that very same Belarus for expensive operations.
Despite the existence of a state program for treating citizens who cannot be helped in Ukraine abroad, they must wait months for a committee’s decision and there aren’t sufficient funds for everyone.

A few years back, the recipients started to speak up. Among them was television journalist and founder of the civil organization the All-Ukrainian Donor Platform iDonor, 31-year-old Iryna Zaslavets. Eight years ago she underwent a bone marrow transplant.
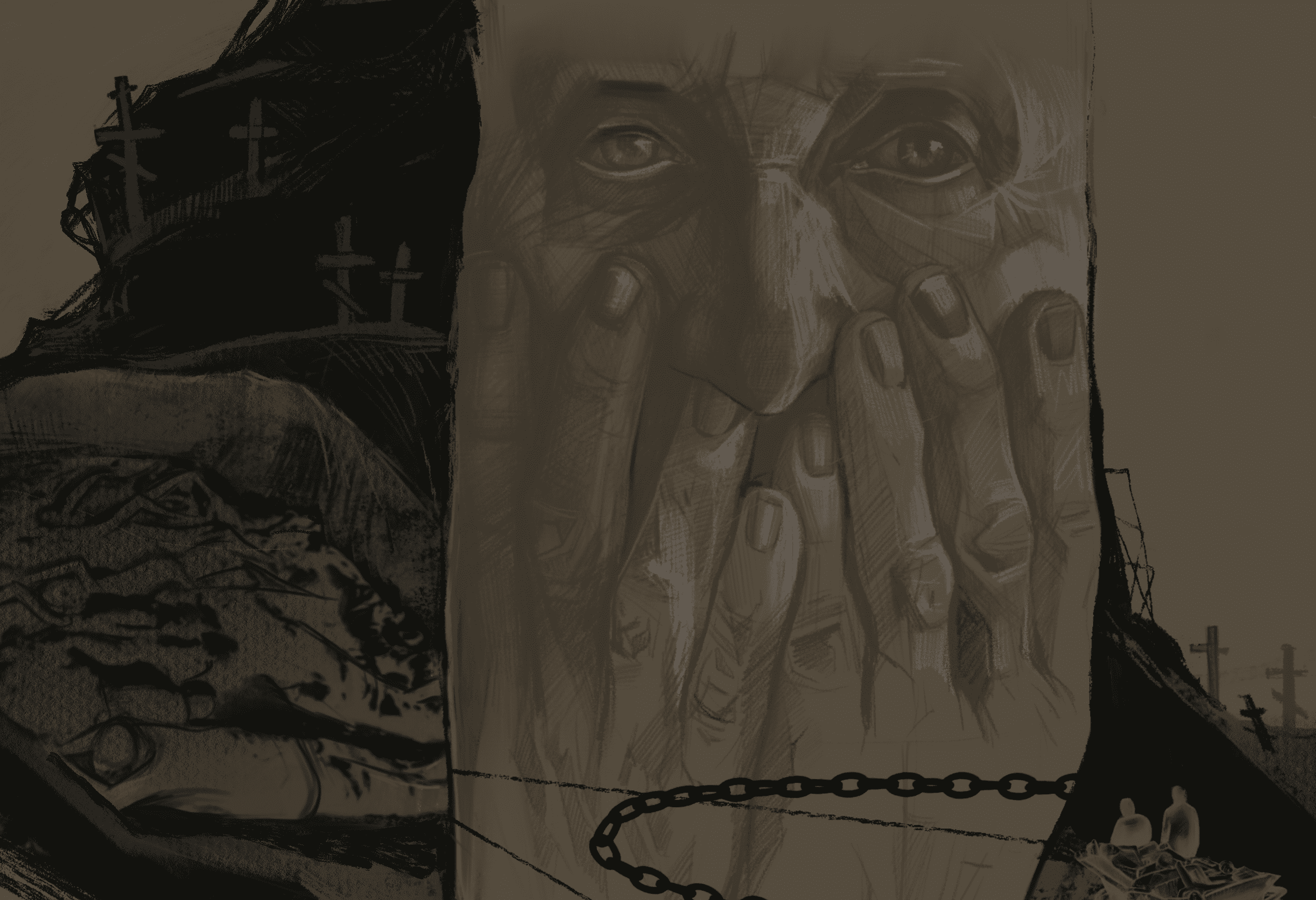
Pray as If You’re Being Heard
“Do you believe in God?” I ask.
She nods.
It’s the early 1990s in the village of Svyrydivka in the Poltava area. After 3-year-old Iryna contracted pneumonia, she developed atelectasis—the collapse of one or both lungs. She was out of breath, gasping at the air, and coughing. After being hospitalized in the regional hospital, her parents were told that both lungs had stopped working and a breathing tube would have to be inserted.
Everytime she was allowed to see her daughter, her mother wailed and fainted.
“Cease these hysterics. The child has pus in her lungs. They have already started to decompose. The child won’t survive,” the doctor prepared her.
An older woman approached her in the hallway.
“You can save your child.”
She gave her a small icon that had the “Our Father” printed on the back.
“Read it not as a poem, but as if you know you’re being heard,” the woman advised.
Oksana Zaslavets prayed all night. In the morning, the surgeon who was supposed to put in the child’s chest stent came. He listened to her breathing for a long time and then sent the girl for an x-ray.
“Mother, you were born under a lucky star. The girl will live—without tubes, without stents, without anything. Her lungs have completely opened,” he exclaimed when he returned with the x-ray.

Later, when Iryna came down with cancer, her family managed to round up 100,000 euros for a transplant and treatment abroad.
“Even if you have money, only one in five survives with my diagnosis and condition a transplant. How could I not believe in God?”
Flowers in Her Chest
In February 2010, Iryna came down with pneumonia again. At that time, she was in her fourth year of studying at the Institute of Journalism at Taras Shevchenko National University in Kyiv, while simultaneously working at the TV stations Culture and City. Her parents decided to take her home for treatment.
Touching her clavicle, she could not figure out where her former hollow had gone. More alarming, her chest cavity was noticeably distended. The patient’s swollen lymph nodes interested the young resident at the district hospital. She dragged out a large medical encyclopedia, started poking her finger around and showing something to the more experienced doctor. They convinced Iryna to go to the district hospital in Poltava.
After a computer tomogram, the doctors there started at the patient as if she were an extinct animal.
“How do you feel? How did you just climb the stairs to the fourth floor?
The exam was not free, but they didn’t ask for any money.
“Don’t worry about it. Believe us, that money’s going to come in handy.”

The radiologist informed Iryna that she had an agglomeration of lymph nodes in her chest the size of a pineapple.
“The local oncologist thrust a needle into the nodes in my neck and under my armpit, took a biopsy, and said, ‘Come back on Monday and we’ll start chemotherapy. You’ll be laid up for four months, but you will live,’” she recalls.
Later on she had a mandatory check-up in the oncology department. The burly man was rough and she was in pain. When she asked him to be gentler, he only said, “You’re not on a date—that would be nice.” Her frightened parents waited in the run-down corridor.
“We left the hospital and walked to the car in silence,” she recalls. “I was in front and my parents behind. I was walking and couldn’t look behind me. It’s so scary when you don’t know what to say.”
Later the doctors in Poltava told them she had Hodgkin’s lymphoma. They advised them to go to Kyiv far from the awful dispensary with the mildew on the walls. Life in the capital led her to the other side of Lomonosov Street—from the student dormitory to the National Cancer Institute.
When Iryna was first at the Cancer Institute, she did not even realize she had cancer. Her parents just kept repeating that it was lymphoma—inflammation of the lymph nodes that is treated with chemotherapy

Hodgkin’s disease is cancer of the lymphatic system. When Iryna was first at the Cancer Institute, she did not even realize she had cancer. Her parents just kept repeating that it was lymphoma—inflammation of the lymph nodes that is treated with chemotherapy.
“Pfft, lymphoma? One-two and we’ve cured it,” the Kyiv hematologist-oncologist waved her hand. Her confidence was calming.
“And I believed them,” Iryna shrugs. “Can you imagine? A 21-year-old journalist with access to the internet. I simply unconsciously agreed to that version of reality. It was easier psychologically.”
It was also easier to forget the doctors.
“I can operate on her tomorrow or in a month,” the surgeon, who was supposed to do the diagnostic operation before starting treatment, told her mom.
He opened his drawer. He hadn’t named a sum, so she tossed in whatever she had.
Later on there was chemotherapy. Her roommate in the hospital room told Iryna to imagine that instead of a tumor growing in her chest, there were flowers growing. That’s what she did.

Some people have a hard time with the “chemicals”—they get nauseous, their head spins, their hair falls out. Chemotherapy kills cells that divide quickly. In addition to cancer, hair follicle cells divide quickly because they are responsible for the growth of hair. Nowadays not everyone loses their hair; the majority of contemporary drugs target only affected cells.
Her chemotherapy lasted all spring and half the summer. It wasn’t too hard on her—she didn’t lose her hair, she felt alive, and even went out dancing. (Only later would she learn that she had the “light” dose of treatment—nobody could have cared less.) The control tomogram showed that the “pineapple” of her lymph nodes had significantly shrunk. This was actually what had been pushing on her heart and lungs, leading to the inflammation.
“Everything’s great, remission. We just need to do radiation to fortify the result,” the doctor said after four cycles of chemotherapy.

The Cancer Institute did not have a linear accelerator. The patients had to wait for one to show up from time to time. They found one at a hospital in Kyiv through a friend in the military. The 89 sessions of radiation with cobalt-60 lasted almost all fall. Sometime then Iryna was fired. “If you get better,” they told her, “come back.”
Winter 2011. A planned follow-up at the Cancer Center.
“It’s back, Iryna. Lymphoma is cured in 9 out of 10 times. Unfortunately you are the tenth,” the hematologist-oncologist told her.
A second opinion at the Lisod private clinic confirmed that the disease had in fact returned.
“Don’t you want to go abroad? I just saw my boss and his acquaintance who treats cancer in Germany was visiting. They’re sending their child there,” her former coworker told her.
The journalist jumped at the chance. She got all the necessary documents together and sent them to a German clinic. They promised to cure her disease just with radiation and presented her with the bill—20,000 euros.
Cheburashka
The diligent Germans did their own research. The results showed that she needed chemotherapy again followed by a bone-marrow transplant, which would cost an additional 100,000 euros. There was a 20% chance Ira would live.

Bone marrow is the soft tissue inside bones that contains hematopoietic (literally “blood building” in Greek) stem cells. They are what make all blood cells. If the disease has infected only the lymphatic system, then before the shock dose of chemicals, they take a portion of the patient’s own, healthy bone marrow. Later they transplant it back so that blood cells can regenerate. This is call autotransplantation. However, if the bone marrow is also infected with lymphoma, they kill it and implant new, healthy bone marrow from a donor who is selected for cellular compatibility.
“In Ukraine, people who are sick believe that the main problem is money. If you find it you will be saved. In reality, in looking for money, we are fighting for the opportunity to fight. And then the doctors give you 60% at first, later 20%.”
Iryna sat and fiddled with the round bead of the gland under her armpit that had been killing her.
“You know, it seems to me, that it’s hardest on friends and family,” she observes. “The person trapped inside her own disease goes through all the stages of grief from denial to acceptance. But friends observe this from the outside and can’t do anything.”
In Germany Ira came to realize just how hard chemotherapy could be. Weakness completely overcame her body. She had to get around in a wheelchair. She could no longer brush her own hair. She would ask others to stroke her head.
In Ukraine, people who are sick believe that the main problem is money. If you find it you will be saved. In reality, in looking for money, we are fighting for the opportunity to fight. And then the doctors give you 60% at first, later 20%.

“Take a picture to remember by. Someday we’ll remember with a smile.”
Her mom waited for a long time and then finally clicked the shutter. Later Iryna would regret taking so few photos. A bald head is a symbol of the fight for life. With her hair cut short and her ears slightly protruding, Iryna’s parents started calling her Cheburashka.
Yet, after two courses of chemotherapy, there were no signs of remission. The doctors decided not to wait and to give her a transplant during her relapse.
May 25, 2011. A bone marrow transplant is like an ordinary blood transfusion, but it takes place within a sterile box—a chamber kept sterile by a special ventilation system that protects against microbes. (After the operation Iryna will live in it for a month while her body is extremely vulnerable.) She gets censors affixed to her from all sides. They brought in the packet with the transplant and emptied its contents into her blood through an IV. The procedure lasted a few minutes.
The complications started a week after the operations, when her blood indices fell suddenly. Since her own bone marrow was being killed, they all dropped to zero. Her lymphocytes—blood cells that fight infection—fell to 0.01%, when 19–37% is normal. Earlier the doctors had noticed that a small piece of one of Iryna’s teeth had broken off, but they had not time to fix it. Microbes, thanks to her near total absence of immunity, started quickly taking over her tooth, which led to hellish pain. She just wanted painkillers.

But then her body started to slowly regenerate. After a month, the doctors let her leave the box and her parents could finally visit their Cheburashka. Later they let Iryna go home, but she remained under the strict supervision of doctors. Her only entertainment during this period was shopping. Armed with bags in case of nausea and smelling salts to prevent loss of consciousness, she and her mom would go to flea markets. They could find good clothes there for 2–3 euros. They wandered among the aisles until Iryna said, “I’m falling.” Her mom caught her under the arms and set her down on the curb.
“I’ll sit here a bit and you go look at that blouse before anyone snatches it up,” the girl pointed and laughed.
Finally she needed radiation. The German doctor sought her information from Ukraine. Iryna laid a small piece of paper with a stamp, “Radiated,” on his desk.
“No, no. You don’t understand,” he stepped out of the office and returned with a thick briefcase containing a load of documents with diagrams and graphs.
“I don’t have anything like that,” she responded.
“There’s no way. Give me the name of your doctor and I’ll find him on the internet.”
“You will never find that major,” she thought.
When the German specialist finds out what device was used for Iryna’s radiation, his head started spinning. It cannot be used on lymphoma. It indicated a low level of education in treating cancer in Ukraine and old procedures. Radiating lymphoma requires a precise calculation of angles and direction of rays in order not to harm healthy cells, whereas in Ukraine not even the dose was recorded. Before she was radiated in Germany, Iryna was “drawn all over like a map of the world.”
Not Why, But What For
After recuperation, her parents tried even harder to hide their daughter from problems. They asked her to stay in her village in the Poltava region for at least a few years. One time she went to church with her mom in Lokhvytsa. There, her mother pointed out a boy who was sick with cancer, Iryna’s peer.
“Remember I told you about him? Could you maybe talk to him?”
It took Iryna a while to gather her thoughts. What should she say to him? That everything would be fine? That’s no fact in Ukraine. Tell him to go abroad? What if he didn’t have the money? But she selected her words and went over to support him. The boy soon died. It is still hard for her to talk about that moment. In psychology this is called survivor’s guilt.

In spring 2012, Iryna returned to Kyiv. Thoughts of “why do I have this disease?” gradually turned into “what for?” She was increasingly presented with opportunities to talk to the sick, who would find her on social media looking for advice and seeking support. That was how she accidentally met Nastia Slipchenko, a young mother sick with leukemia. They wouldn’t accept her at the hospital since the death of cancer patients ruins their stats. When she was tormented with severe pain, an ambulance would come to give her an injection of No-Spa (drotaverine) and take off.
The money for Nastia’s bone marrow transplant came too late. She was airlifted to Germany, but her disease had already metastasized to her brain. All the doctors could do was give her a large quantity of pain killers so she could die in peace.
“Nastia’s death was a terrible blow. For a long time my feeling of guilt prevented me from talking to other sick people because there was nothing I could do to help them. But I had an inner need to do something important,” Iryna says.
In summer 2013 she landed on the STV channel on their News Window segment. With a group of colleagues, she had started working with the Ukrainian Charity Exchange—the first independent social service for online charity in Ukraine. They prepared stories about people who needed money for medical treatment. It turned out that charity is not only transaction information, but also a bunch of risks, inspections, and paper trails.
“But when you see on the site how people are giving money and “collected” lights up after the story comes out, it fills you with an unbelievable feeling of happiness. Someone has just gotten a chance at survival.

In her stories on STV, Iryna Zaslavets also shared information about a state program to treat Ukrainian citizens abroad—those whom the state cannot save at home. It is an annual program, but doctors don’t publicize its existence.
“A doctor told a sick person I know, ‘Don’t be a fool, no one’s going to give you money.’ But she didn’t listen and got her documents together, and she’s already been operated on in Belarus,” Iryna says.
When you see on the site how people are giving money and “collected” lights up after the story comes out, it fills you with an unbelievable feeling of happiness. Someone has just gotten a chance at survival
Last year the Ukrainian Ministry of Health put 389 million hryvnias toward this program and by summer the money was all gone. At first the relatives of people with cancer protested near the Verkhovna Rada, but later they took their tents to the Ministry of Health where they camped out for a few months. Subsequently the amount was increased to 654 million until the end of the year. For this year the MoH has again set aside 389 million hryvnias, but under pressure from activists the deputies increased the program’s budget nearly twofold.
Finally, after two years of actively shedding light on this topic in the media, the government have admitted that it would be more effective to develop their own system for transplants than finance expensive transplants abroad. In May 2018, the deputies approved a law that would stimulate the development of a postmortem organ-donation program. A single donor can save up to eight lives: two lungs, two kidneys, a heart, liver, pancreas, and intestines. But the new law only tied doctors’ hands.

“It is overladen with details. And at the same time, putting it into effect is expensive and protracted: you need to create donor and recipient registries, prepare transplant coordinators, purchase equipment to diagnose brain death,” Iryna explains.
Postmortem organ donation is only possible after proving brain death. The heart can keep working, all vital functions of important organs will continue, but blood is not going to the brain, for example, because of edema. Most often this happens as a result of a craniocerebral injury. Unlike clinical death, this is an irreversible process since brain cells do not regenerate.
Brain death is diagnosed by special sensors that detect gas (if there isn’t any oxygen in the brain, it is dead) and a series of additional methods that are applied over two days. Ukrainian hospitals today are not provided with this equipment. And it is literally necessary not only to identify potential donors, but also for treatment itself. It happens that patients are kept on ventilators and given expensive drugs on their relatives’ dollar because they simply cannot determine brain death. The person seems to be alive, but has in fact already died.
“It’s not clear why, in the law, the transplant coordinator can only be an anesthesiologist,” Iryna criticizes the new law. “In India, for example, there is a ‘grief counselor’ who communicates with the families of the potential donors. Not doctors, since the families could suspect them of pressuring them. Often they’re volunteers who have lost relatives because an organ wasn’t available or who were themselves saved by a transplant. As a rule, the families of the potential postmortem donor are in a state of sorrow or anger. The psychologically wrong type of communication could just make the families get angry and kick the doctor out.”In India Iryna filmed a series of reports called Heart Failure where Ukrainians who were operated on there speak, in particular, about the culture of organ donation there.
A single donor can save up to eight lives: two lungs, two kidneys, a heart, liver, pancreas, and intestines

“They have memorial plaques to donors who haven posthumously given the gift of life to so many people. The police make ‘green corridors’ so the ambulances with the transplants can get through without traffic. And the people who get stuck in jams as a result, rather than getting mad, throw flowers at the ambulances.
The transplant law was supposed to go into effect January 1, 2019. But when the day came, the registry was not ready and neither were the transplant coordinators. Doctors, fearing criminal responsibility, ceased conducting even familial transplants since the new law required absolutely all donors and patients be registered. Finally, under pressure from activists, deputies managed to postpone the action of a certain of the law’s provisions until next year.
Building Bridges
The hematologist-oncologist at the National Cancer Center, Yevhen Kushchevy, is bothered by the media’s and society’s sudden interest in the problem of bone marrow transplants.
“The shame is that it’s often ignoramuses making noise,” he says. “They’re screaming about the necessity for sterile boxes and waiting lists, but that’s not the main problem. An allogeneic bone marrow transplant is one of the most difficult complex treatments in the world.”

Donor bone marrow is transplanted so that the patient can fight their tumors. Yet it’s also fairly common for the host to reject the transplant. This is one of the main causes of death in patients after an allogeneic transplant. Of course, when a donated organ is transplanted, the recipient’s immunity begins to attack it as a foreign body; therefore it has to be suppressed by various special drugs. But bone marrow transplants are even more complicated since, in essence, the recipient is being given a foreign immunity in hopes that it will begin to fight the tumor as if it were native. Instead, the transplanted immunity can begin to attack not the tumors, but the body of the patient herself. The doctor here must essentially walk on a tightrope: the more immunosuppressors, the greater the risk of relapse of the disease; fewer immunosuppressors, the greater the risk that the transplant will kill the host.
In order to prevent this, you need a laboratory that can precisely measure the concentration of immunosuppressors in the blood and diagnose various immunological complications. Besides that, every transplant center has to have its own highly developed microbiology lab, since infections that are already present in the body and are usually suppressed by the immune system can kill a patient after a bone marrow transplant.

“Yet another problem is doing radiation after a bone-marrow transplant,” Kushchevy continues. “In Ukraine no one can yet properly do total body irradiation. In order not to kill the patient with radiation, the doctor is supposed to go through education at a clinic that has many years of experience. Patients can often die from complications, which is why therapy here is often reduced, made less aggressive because we’re not capable of dealing with complications. Accordingly, it is less effective. Hence our survival rates are much worse than in the rest of the world. Lots of hospitals still follow procedures from 30–40 years ago.”
Studying the topic of transplants for more than two years, Iryna has come to understand the that parallel worlds of doctors, patients, and functionaries do not intersect.
“I realize that I could build bridges,” Iryna explains. “Help them listen to each other. That’s when I decided to start a community organization in order to popularize the culture of organ donation and facilitate the creation in Ukraine of an active transplant system. We called it iDonor since every individual can become a donor and save others.”

Last year, together with the MoH, iDonor organized a large conference that brought together doctors, patients, local authorities, and functionaries. They conducted a survey, during which it was revealed that only 10% of doctors surveyed believed that transplants in Ukraine could start happening that year (2018), and 80% hoped it would be possible within 5 years.
Iryna is also a member of a group of experts from the MoH on transplant questions. She has identified four main directions for the development of transplants in Ukraine: equipment for the mandatory diagnosis of brain death, legal defense for all sides in the process, filling out the registries and debugging transplant coordination services, and an uninterrupted supply of immunosuppressors for recipients.
Today Ukraine has started training its first transplant coordinators. It is they who will set up the interactions between all the participants in the transplant process—consents to donate, quick and safe organ transport, the timely filling of the Single State Transplant System, which was presented in April of this year and is currently being tested in the MoH. The transplant coordinators will register all donor and patient parameters, and the system will automatically find the optimal matches without human intervention.
I realize that I could build bridges. Help them listen to each other. That’s when I decided to start a community organization in order to popularize the culture of organ donation and facilitate the creation in Ukraine of an active transplant system. We called it iDonor since every individual can become a donor and save others

It is also important how people end up on the donor list. In the US, for example, all citizens indicate their position on postmortem organ donation when they receive their driver’s licenses. In Ukraine, you can theoretically inform your family physician about your consent or refusal to donate, or appoint a responsible person in case of your own death.
Iryna Zaslavets ended the last episode of Heart Failure with the following words, “I, Iryna Zaslavets, in the case of my death, bequeath my organs to doctors with the hope that they will prolong someone’s life.”
Translated by Ali Kinsella.
[This publication was created with support of the Royal Norwegian Embassy in Ukraine. The views and opinions expressed in this publication are those of the authors and do not necessarily reflect the official position of the Norwegian government].
Have read to the end! What's next?
Next is a small request.
Building media in Ukraine is not an easy task. It requires special experience, knowledge and special resources. Literary reportage is also one of the most expensive genres of journalism. That's why we need your support.
We have no investors or "friendly politicians" - we’ve always been independent. The only dependence we would like to have is dependence on educated and caring readers. We invite you to support us on Patreon, so we could create more valuable things with your help.
Reports119
More